Treatment of hypokalemia
Overview
Normally, blood potassium level is 3.5 to 5.5 mEq/L or mmol/L (1 mEq = 1 mmol potassium). Hypokalemia is usually defined as a serum potassium level ≤ 3.5 mmol/L. Up to 21% of hospitalized patients develop hypokalemia during their stay, with 5.2% being classified as severe (< 3.0 mmol/L). Up to 40% of outpatient treated with diuretics suffer from hypokalemia.
Causes of hypokalemia
- Medication use such as laxatives and diuretics.
- Low potassium intake.
- Gastrointestinal (GI) potassium loss caused by diarrhea and vomiting.
- Renal potassium loss caused by diuretics (are the most common medications associated with hypokalemia), hyperaldosteronism, cushing disease, licorice ingestion), hypomagnesemia and metabolic alkalosis.
Assessment
Symptoms and signs
Correlate with the degree of hypokalemia as well as with the rate of decline of plasma potassium. They include musculoskeletal (myalgias, weakness, and paralysis), GI (nausea, vomiting, constipation, and ileus), cardiovascular (palpitations, ECG changes, and arrhythmias), renal (polyuria), and CNS (mental status changes). Patients with underlying cardiac disease or hypertension are more likely to experience cardiac arrhythmias from hypokalemia.
With mild hypokalemia (3 - 3.5 mmol/L), patients are often asymptomatic. With moderate hypokalemia (2.5 - 3 mmol/L), patients may experience ECG changes (flat or inverted T waves, U waves, ST depression), fatigue, myalgias, or GI symptoms (constipation, nausea, and vomiting). With severe hypokalemia (2 - 2.5 mmol/L), patients may experience ascending muscle weakness, ileus, more severe ECG findings. Critical hypokalemia (< 2 mmol/L) — rhabdomyolysis, respiratory failure, arrhythmias, and even death are life- threatening complications that can occur from critically low serum potassium.
Treatment
Mild hypokalemia (3.0-3.5 mmol/L)
Initially start with increasing dietary potassium intake (such as oranges and bananas) and consider beginning oral potassium supplementation. Oral dietary or pharmacologic potassium supplements are used for mild hypokalemia.
Oral potassium therapy ㅡ Potassium chloride is default and preferred salt choice, start by 40-100 mEq PO daily in divided doses; single dose not to exceed 25 mEq to minimize GI discomfort (must be taken after meals). Aternatively, 10-20 mEq PO BID/QID (20-80 mEq/day). While potassium bicarbonate is indicated for patients with hypokalemia and metabolic acidosis (pH less than 7.4). Potassium phosphate may be indicated for patients with phosphate deficits (as in diabetic ketoacidosis).
Moderate hypokalemia (2.5-3.0 mmol/L)
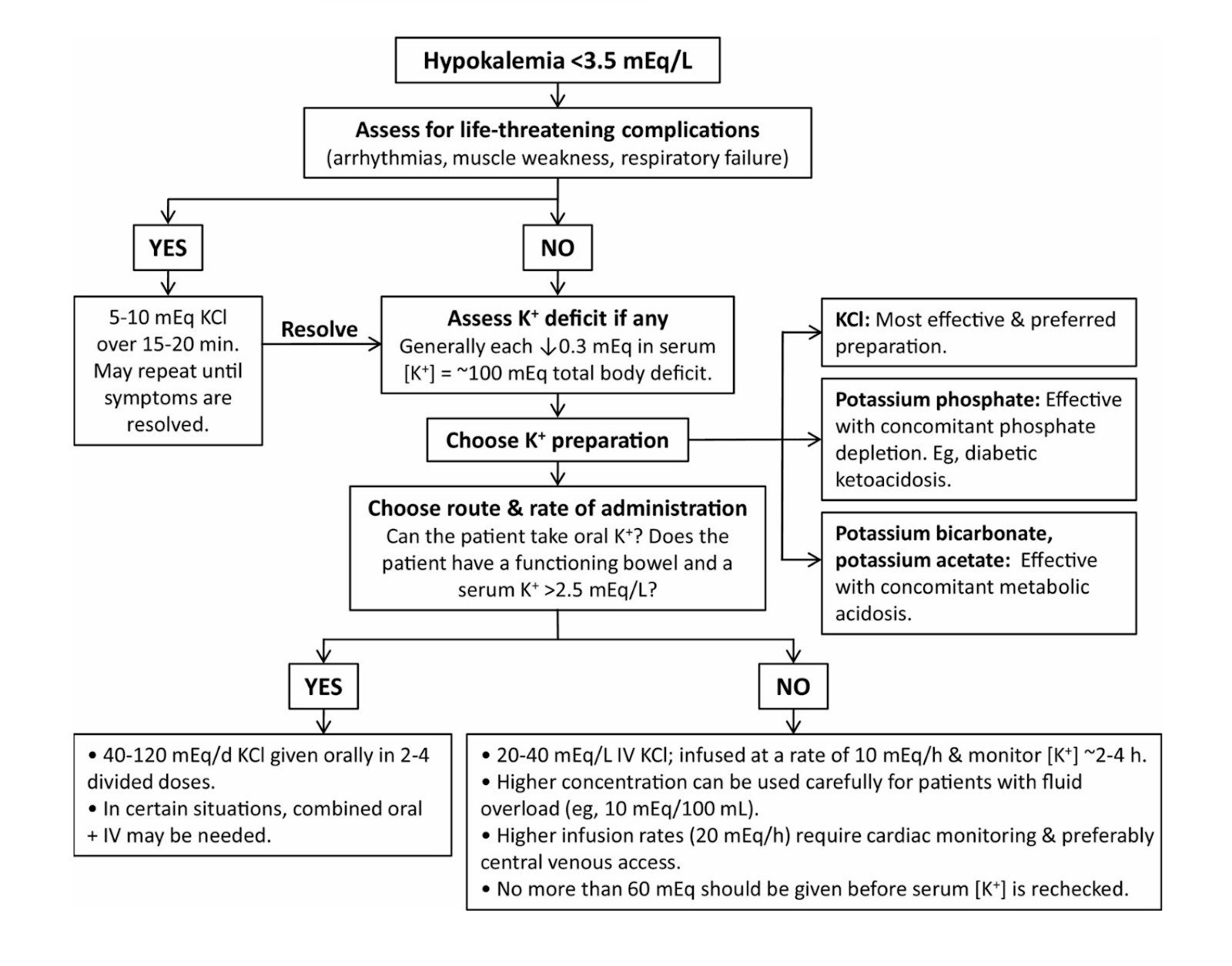
Consider oral potassium supplementation. If symptoms are severe, recommend IV therapy, "see algorithm and table 1 for summary of hypokalemia treatment". Hypokalemia from diuretic use (mild to moderate) can be treated by oral potassium supplementation is often necessary and adding a potassium-sparing diuretic (spironolactone 25 mg daily) is often useful.
Severe hypokalemia (< 2.5 mmol/L)
Treat with IV therapy as inpatient, with cardiac monitoring. Especially consider empiric magnesium replacement in refractory hypokalemia. Magnesium sulfate is 10% (1 gram Magnesium per 10 mL solution) and can be given by dose 1-2 g slow IV (diluted in 50-100 mL D5W) over 5-60 minutes.
Intravenous potassium therapy ㅡ IV potassium chloride saline solution is used for severe (less than 3.0 mEq/L) symptomatic hypokalemia or for hypokalemia associated with life-threatening ECG changesIn patients with significant dysrhythmias (eg, ventricular tachycardia) as a presenting symptom, 20 mEq IV potassium chloride can be pushed over 3 to 10 minutes to prevent deterioration into cardiac arrest. Dosing and infusion rate recommendations vary; central-line infusion and continuous ECG monitoring highly recommended for infusions >10 mEq/hour.
| Table (1). Treatment of hypokalemia | ||
|---|---|---|
| Hypokalemia | Treatment | Comments |
| Mild (3.0–3.4 mEq/L) | Potassium tablets (72 mmol/day) or i.v. potassium infusion 25 mL (75 mmol/day) |
|
| Moderate (2.5–2.9 mEq/L) | Potassium tablets (96 mmol/day) or i.v. potassium infusion 25 mL (100 mmol/day) |
|
| Severe (< 2.5 mEq/L or symptomatic) | Intravenous replacement 40 mmol KCl in 1 L 0.9% NaCl (glucose 5% may be used, but NOT preferred) |
|
Dosage of IV potassium therapy
- Serum potassium 2.5 to 3 mEq/L: Initial: 10 to 20 mEq/hour and adjust based on frequent serum potassium monitoring; maximum infusion rate: 20 mEq/hour with continuous ECG monitoring.
- Serum potassium < 2.5 mEq/L or life-threatening hypokalemia (not for emergency treatment of cardiac arrest): Initial 10 to 40 mEq/hour and adjust based on frequent serum potassium monitoring; maximum infusion rate (central line only) is 40 mEq/hour with continuous ECG monitoring; some patients may require up to 400 mEq/24 hours.
- Dilute potassium ampoules in normal saline NOT in 5% glucose.
References
- Viera AJ, Wouk N. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2015 Sep 15;92(6):487-95.
- Asmar A, Mohandas R, Wingo CS. A physiologic-based approach to the treatment of a patient with hypokalemia. Am J Kidney Dis. 2012 Sep;60(3):492-7.
- Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocr Connect. 2018 Apr;7(4):R135-R146.