Assess the need for SEIZURE prophylaxis
Guidelines for seizure prophylaxis post-neurological injury, trauma, TBI, ICH, and SAH....
As a critical care pharmacist, questions are still popping up about seizure prophylaxis after a neurological injury, trauma, intracranial hemorrhage, etc.
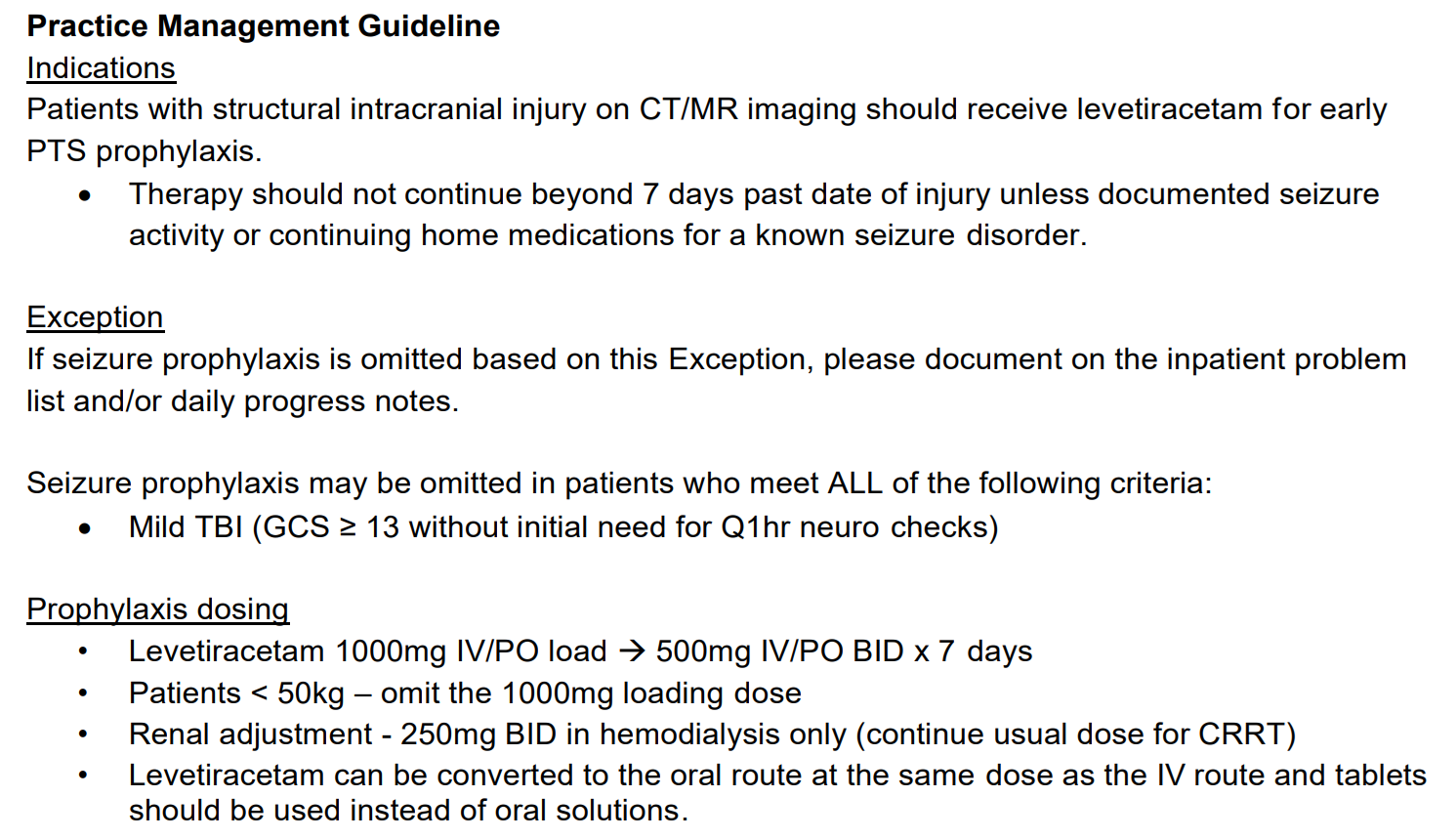
- Who should get it? Continue to use seizure prophylaxis after a SEVERE traumatic brain injury (TBI); Glasgow Coma Scale 3 to 8. About 1 in 10 TBI patients have seizures and prophylaxis can reduce occurrence in the first week. Don't routinely give seizure prophylaxis after an intracerebral hemorrhage (ICH) or subarachnoid hemorrhage (SAH). There's no consistent benefit, and limited data suggest worse outcomes. But don't be surprised if specialists use it in some ICH or SAH patients, there's debate about whether certain patients may benefit. For example, it may be started due to a bleed in the temporal lobe.
- What should you give? Both phenytoin and levetiracetam seem to decrease early seizures. Lean toward levetiracetam for fewer side effects and interactions. Start ASAP, many seizures occur in the first 24 hours. You don't need to load levetiracetam due to its shorter onset and half-life. But do consider loading if using phenytoin. Generally stick with standard doses, such as levetiracetam 500 mg to 1,000 mg BID and give orally, if able. If IV levetiracetam is used, ask about incorporating IV push maintenance doses to improve efficiency, instead of piggybacks.
- When should you stop? Generally, stop seizure prophylaxis after 7 days, or sooner for SAH if the aneurysm has been secured. Think about adding a stop date to your document. Or put seizure prophylaxis on your list of meds to assess at discharge or transfer. These are often continued longer than intended.
NPS-adv
References
- Khan NR, VanLandingham MA, Fierst TM, et al. Should Levetiracetam or Phenytoin Be Used for Posttraumatic Seizure Prophylaxis? A Systematic Review of the Literature and Meta-analysis. Neurosurgery. 2016;79(6):775-782.
- Angriman F, Tirupakuzhi Vijayaraghavan BK, Dragoi L, Lopez Soto C, Chapman M, Scales DC. Antiepileptic Drugs to Prevent Seizures After Spontaneous Intracerebral Hemorrhage. Stroke. 2019;50(5):1095-1099.
- Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711-1737.
- Hemphill JC 3rd, Greenberg SM, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032-2060.