Manage HYPERglycemia in hospital
Strategies for achieving glycemic control and hyperglycemia management in non-critically ill hospitalized patients.
Introduction
Hyperglycemia was defined as a fasting or admission blood glucose > 126 mg/dL or a random blood glucose > 200 mg/dL. Serum blood glucose control should be done with basal and bolus insulin, with additional coverage with slide scale (correction insulin). Avoid sliding scale insulin alone as it associated with worse outcome.
NPS-adv
Glycemic control
Benefits of glycemic control using continuous intravenous insulin infusions include decrease hospital mortality rate, decrease rate of bacteremia, multiorgan failure, surgical site infections, and recurrent ischemia and lower incidence of renal failure, or need for renal replacement therapy.
| Table (1). Glycemic Goals | ||
|---|---|---|
| ADA | AACE | |
| Intensive care setting | Goal < 110 mg/dL; Maximum < 140 mg/dL | 80-110 mg/dL |
| Non-critical care setting | Preprandial < 126 mg/dL | Preprandial < 110 mg/dL |
| Postprandial < 180-200 mg/dL | Postprandial < 180 mg/dL | |
| Abbreviations: ADA, American Diabetes Association; AACE, American Association of Clinical Endocrinologists. | ||
Strategies of glycemic control
All oral hypoglycemics were discontinued on admission...
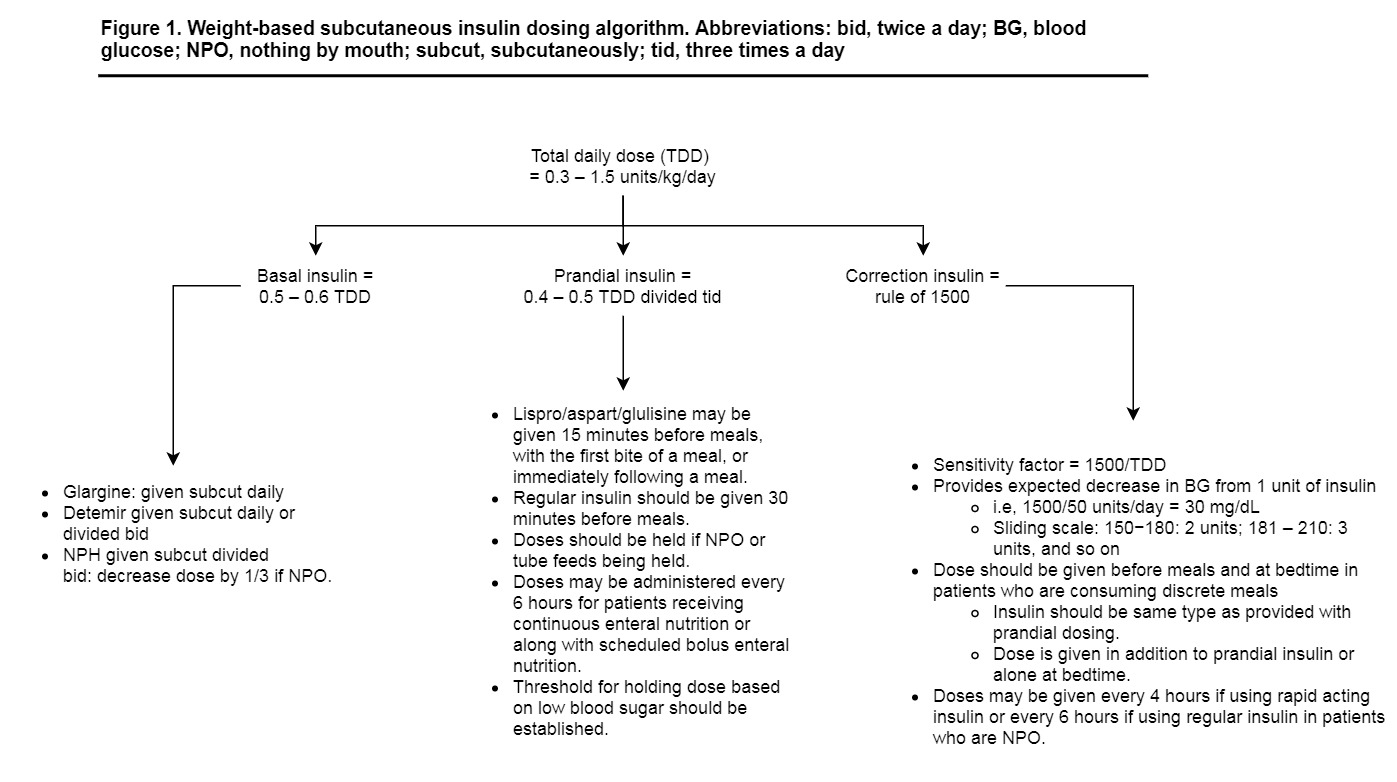
- Basal-bolus method ㅡ Basal-bolus therapy is to mimic normal physiology. Involve basal, bolus or prandial, and correction insulin. Basal insulin is provided with a long-acting agent such as glargine or detemir, or an intermediate acting agent such as NPH. Basal insulin should be provided to all type I diabetic patients to prevent ketoacidosis and to all hyperglycemic patients who are consistently requiring correction therapy. Bolus or prandial insulin is used prior to meals to help minimize elevations in blood glucose secondary to dietary carbohydrate intake. Correction insulin is provided in addition to scheduled insulin to account for preexisting hyperglycemia before meals and at bedtime.
- Basal insulin: long-acting Insulin (e.g. Lantus, NPH). Do not adjust Lantus for oral intake (it is not recommended to decrease or withhold the dose if nutrition is suspended). NPH may require adjustment if covering mealtime - it is recommended to decrease the usual dose of NPH by 1/3 (ie, give 2/3 of the usual dose) when nutrition is withheld.
- Bolus insulin: rapid-acting (e.g. Lispro, Aspart and Glulisine). Cover meals, snacks with units per carbohydrate. Glulisine, Lispro, and Aspart provide better postprandial control than regular insulin (Actrapid).
- Insulin dosing in basal-bolus method ㅡ The usual range for total daily insulin requirements is 0.3 to 1.5 units/kg/day. Most patients will fall into the range of 0.5 to 0.7 units/kg/day. For patients with blood glucose of 140 to 200 mg/dL, insulin therapy was started at 0.4 units/kg. For patients with blood glucose of 201 to 400 mg/dL, insulin was started at 0.5 units/kg.
- OR, simple method for total daily dose (TDD) of insulin.
- Stage IV chronic kidney disease, not on hemodialysis: start 0.25 units/kg.
- Underweight (advanced age, hemodialysis): start 0.3 units/kg.
- Normal weight: start 0.4 units/kg.
- Overweight: start 0.5 units/kg.
- Obese (or insulin resistant, on systemic corticosteroids): start 0.6 units/kg.
- The glargine dose consisted of one-half (50%) of the total daily dose (TDD) of insulin; glulisine accounted for the other one-half (50%) and was given in 3 equally divided doses before meals. If patients were not eating discrete meals, glargine was administered and glulisine was held. In patients who are receiving combination insulin preparations (mixtures of intermediate and rapid or short-acting insulin), it is recommended to convert these patients to long-acting basal insulin plus short or rapid-acting prandial insulin during hospitalization to allow ease in dose titration. Figure (1). Weight-based subcutaneous insulin dosing algorithm.
- Correction insulin ㅡ Correction, or supplemental, insulin in addition to scheduled prandial and basal insulin should be made available in an adjustable fashion to correct preexisting mealtime and bedtime hyperglycemia. This is provided in addition to meal time insulin or alone at bedtime or if a patient is not receiving nutrition. The same type of insulin should be used for both prandial and correction dosing (i.e. Lispro, Aspart and Glulisine). To calculate dose of correction insulin, it is recommended to first calculate sensitivity factor (SF) of the patient to insulin...
- A sensitivity factor (SF) is a marker of how much a patient’s glucose level will decrease, given 1 unit of insulin.
- The SF is determined by dividing 1500 by the TDD.
- For example, a patient with a TDD of 50 U would have SF of 30 (1500/50 = 30), meaning that 1 unit of insulin would be expected to decrease the blood glucose by 30 mg/dL.
- Correction orders should start at a threshold that is safe for the patient to receive when they are not receiving nutrition. Typically, correction orders begin when the blood glucose is above the identified glycemic target (i.e., >150 mg/dL).
- Correction orders should start at 2 units and increase by 1 unit for every increment of the SF. Using the example mentioned earlier, a meal time blood glucose correction scale would include the following: 150 to 180 mg/dL give 2 units, 181 to 210 mg/dL give 3 units; 211 to 240 mg/dL give 4 units, and so on..
References
- Arnold, L.M., Keller, D.L. and Tofade, T.S. (2009). Hyperglycemia Management in Non-critically Ill Hospitalized Patients. Journal of Pharmacy Practice, 22(5), pp.467–477. Available at: https://doi.org/10.1177/0897190008330198.